Proper testing can help to prevent the placement of any of a number of materials in the mouth that could prove to be an ongoing source of toxins to a patient.

Dental toxicity can occur when materials placed in a patient’s mouth cause that person’s immune system to react and “reject” the restoration since the components are never accepted in the same manner as one’s own tissues. This is probably one of the primary concerns facing dental patients today. With several thousand dental restoration materials available on the market, it is important to know how vigorously or minimally these materials will react with the body’s immune system. Serum compatibility testing provides dentists with one way to help determine which materials will react in a test tube with a patient’s serum proteins, and to what extent this will happen. Proper testing can help to prevent the placement of any of a number of materials in the mouth that could prove to be an ongoing source of toxins to a patient.
Reactivity to dental materials can be loosely compared to food allergies. While many people have no problems with foods such as peanuts, fish, or soybeans, there is a small percentage of the population who will have an allergic reaction to these foods. The reaction to dental materials that we are testing for is similar to an allergy, but it appears to often be much more subtle. Most people do not even notice that anything is happening since they experience no immediate symptoms, but there can still be a reaction taking place. The immune system can react to dental materials as if they were infections or just toxic substances, and it will begin to work overtime to remove the “infection” from the body, although this can obviously never occur as long as the substances remain in the mouth. Often these materials are placed with no investigation into potential problems because the dentists themselves are unaware of the hazards.
While no ethical dentist would ever knowingly place a toxic material in a patient’s mouth, most are simply unaware of the danger. Very few dentists are ever taught that patients can have a reaction to dental work, and those who are educated often believe that only certain types of materials are reactive, and that by avoiding them, they can avoid any such problems. The truth is that anybody can have an immune reaction to any material, and one very good way to minimize the possibility of such problems is to test the body’s reactions in vitro (in a laboratory) via Serum Biocompatibility Testing.
While there are thousands of materials available for use in dental restorations, there are three major types of material: metallic, composite and ceramic.

Metallic components include both amalgam materials and casting alloys. Amalgams are used primarily as filling materials, and casting alloys find use in crowns and bridges, as bases for ceramic restorations, and in orthodontic work.
The first and perhaps the most talked about types of dental restoration materials are amalgam fillings. An amalgam is obtained by mixing mercury with other metals; this mixture can then be used to fill a cavity. The mixture is often liquid or very near to a liquid at room temperature, so it can easily form to the contours of a cavity and fill the space very effectively. Recently, an increasing number of patients are moving away from amalgam fillings for a variety of reasons: some for aesthetic reasons, others because of concerns about the mercury content or concerns over metallic components in general.
Many other dental restorations use gold or other precious metal-based casting alloys, and are most commonly used in crowns. While pure gold is much too soft to make effective dental restorations, it has many other properties that make it an ideal starting material for dental alloys. Several other metals are commonly mixed with gold in order to obtain an alloy that combines the most favorable properties of each metal. Gold and platinum are often selected because they are resistant to tarnish and corrosion and often demonstrate only very minimal immune reactivity in the biocompatibility testing. Metals like copper and palladium are used to modify the color of the alloy, while others such as silver and iridium are used to give the alloy more strength. There are even more metals that are used in dental work to alter melting points, hardness, color, and the durability of alloys. Any given alloy could have up to a dozen different component metals, so it is important to know which metals you will substantially react to before they are placed in the mouth.

Composite materials, commonly known as “white fillings,” are one type of dental material that is quickly gaining popularity. These are a type of glass-plastic material, often selected for aesthetic reasons because they can be made to look just like a real tooth. Many patients prefer composite fillings because they are sensitive to the other types of fillings available. Perhaps the most common misunderstanding about composite fillings is that they are all the same. Actually there is a wide variety of component chemicals that can be used to make composites, allowing a dentist to use precisely the right material for any situation.
The plastic portion of the composite is a polymer, a large molecule that is made up of many smaller molecules called monomers. These monomers are usually a type of dimethylacrylate that is able to form long chains, as well as links between chains to form a very stable polymer matrix, like a spider’s web, that will not dissolve in water. Inside the polymer matrix is some sort of glass filler material. Quartz, borosilicate, silicon dioxide, and barium glass are among the more commonly used materials for this purpose. These fillers keep the composite from expanding or shrinking, prevent water absorption, and make the plastic stronger. Some composites also contain catalysts and accelerators to make the plastic portion set more quickly and effectively. Methacrylic acid and colloidal silica can also be added to the mixture to obtain a faster setting and stronger filling. Finally, a surface treatment is used to link the polymer and the filler together. Since there are many different options for each component, and not every component is used, there are literally thousands of possible combinations of chemicals that can make a composite material.

Porcelain and ceramic materials are popular as dental restoratives because they look and feel very much like real teeth. It is difficult to provide a comprehensive list of ceramic components since they vary greatly depending, not only on the materials used but also depending on the type of restoration. The basic ceramic restoration consists of the exterior restoration, which is fused to a framework. The framework is then attached to the teeth in order to hold the prosthetic in place. The exterior can be cut or milled from a prefabricated block of material, or it may be built up layer by layer to give the proper shading and appearance of a real tooth. It is then fired in order to harden the material and fuse the ceramic to the framework. The framework can be either a metal alloy (often gold based), or a sturdier form of ceramic. The exterior ceramic is usually a type of porcelain made up of silicon dioxide, and typically containing varying amounts of zirconia or alumina to give it the proper color. Ceramic restorations can contain far more ingredients than those listed above, and the variations in composition give the wide range of properties that any given material can produce. The framework of a ceramic restoration can be made from metal or another form of ceramic. The metal is usually an alloy of gold, platinum, palladium and silver, although many other metals are often used. A ceramic framework generally has a high zirconia content and can contain any of the same components as the exterior material.

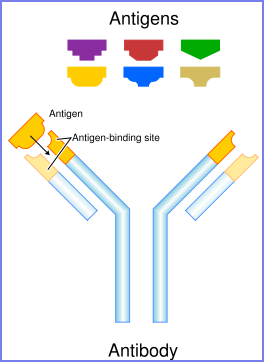
The human immune system is one of many methods that the body has to protect itself from harm. It works by recognizing substances that do not belong in the body and removing them. Such substances are called antigens and may include viruses, bacteria, fungi, toxins, and parasites. Immunologists describe two general types of antigens: those that are supposed to be present in the body are called “self” antigens, while those that are not supposed to be there are called “non-self” antigens. Recognition and removal of antigens is handled by about a dozen specialized cell types collectively known as white blood cells or leukocytes. It is theoretically possible for anything to create an immune response. All that needs to happen is for the immune system to recognize the substance, and the immune system can recognize any antigenic substance.
Many of the metals and components of composite materials are part of a group of chemicals called haptens. These are atoms or small molecules that do not prompt an immune response themselves, but they can combine with a carrier, a larger molecule (usually a protein) in the body, to form a substance that will trigger the immune system. If the carrier is a self antigen then there is a possibility that the immune system will begin to recognize the carrier without the hapten. This results in an autoimmune disease, where the immune system attacks part of the body as if there were an infection. These types of immune reactions have been linked to diseases such as multiple sclerosis and lupus erythematosus.
The presence of dental or other toxins in the body is easy to detect by the elevated levels of lymphocytes and other components of the immune system. One would expect to see similar elevations in a person suffering from a cold or flu. These elevations indicate that the immune system is actively fighting an infection. The difference is that with a cold or flu, the immune system can eventually rid the body of the infection. With dental toxicity, the source of the problem is permanently imbedded in the mouth and only the chemicals that are released into the body can be dealt with. This keeps the immune system on “alert” status all the time, while simultaneously using a significant portion of the body’s nutrients and energy in order to maintain this level of activity.
Many of the metals and components of composite materials are part of a group of chemicals called haptens. These are atoms or small molecules that do not prompt an immune response themselves, but they can combine with a carrier, a larger molecule (usually a protein) in the body, to form a substance that will trigger the immune system. If the carrier is a self antigen then there is a possibility that the immune system will begin to recognize the carrier without the hapten. This results in an autoimmune disease, where the immune system attacks part of the body as if there were an infection. These types of immune reactions have been linked to diseases such as multiple sclerosis and lupus erythematosus.
The presence of dental or other toxins in the body is easy to detect by the elevated levels of lymphocytes and other components of the immune system. One would expect to see similar elevations in a person suffering from a cold or flu. These elevations indicate that the immune system is actively fighting an infection. The difference is that with a cold or flu, the immune system can eventually rid the body of the infection. With dental toxicity, the source of the problem is permanently imbedded in the mouth and only the chemicals that are released into the body can be dealt with. This keeps the immune system on “alert” status all the time, while simultaneously using a significant portion of the body’s nutrients and energy in order to maintain this level of activity.
Serum Biocompatibility Testing

Serum Biocompatibility testing was developed to determine how much of an immune reaction a particular client will have to any given material. A blood sample is drawn and spun on a centrifuge in order to separate the blood cells from the blood serum. The cells are discarded and the serum, which contains all of the free-floating antibodies and other blood proteins, is collected for testing. A small sample of the serum is then mixed with the individual chemical components that may be found in dental materials. If the chemicals would cause an immune reaction in the body, then the antibodies present in the serum will bind the chemicals and form an antibody complex making the mixture look cloudy.
This is known as a protein fallout reaction. A simple but elegant machine called a light densitometer is then used to measure the opacity of each serum-chemical mixture, and the chemical is then judged according to protocols originally developed by Dr. Hal Huggins and refined over decades of testing. For the dentist’s convenience the classifications “Highly Reactive,” “Moderately Reactive,” and “Least Reactive,” are used to aid in understanding the results. Each product on the test is then rated by the highest reactivity level among its component chemicals. This assures that only the products in which all components give the lowest reaction levels are termed “Least Reactive.”
